All the body’s systems and organs are important to its proper functioning, but in an emergency situation, medical professionals focus their evaluation on particular systems and structures for the purposes of triage and keeping patients stable until they can receive treatment.
The most commonly used approach for trauma assessment is usually referred to as the ABCs of trauma: Airways, Breathing, and Circulation. Additional letters (such as D and E, which cover neurological disability and exposure, respectively) are also sometimes added.
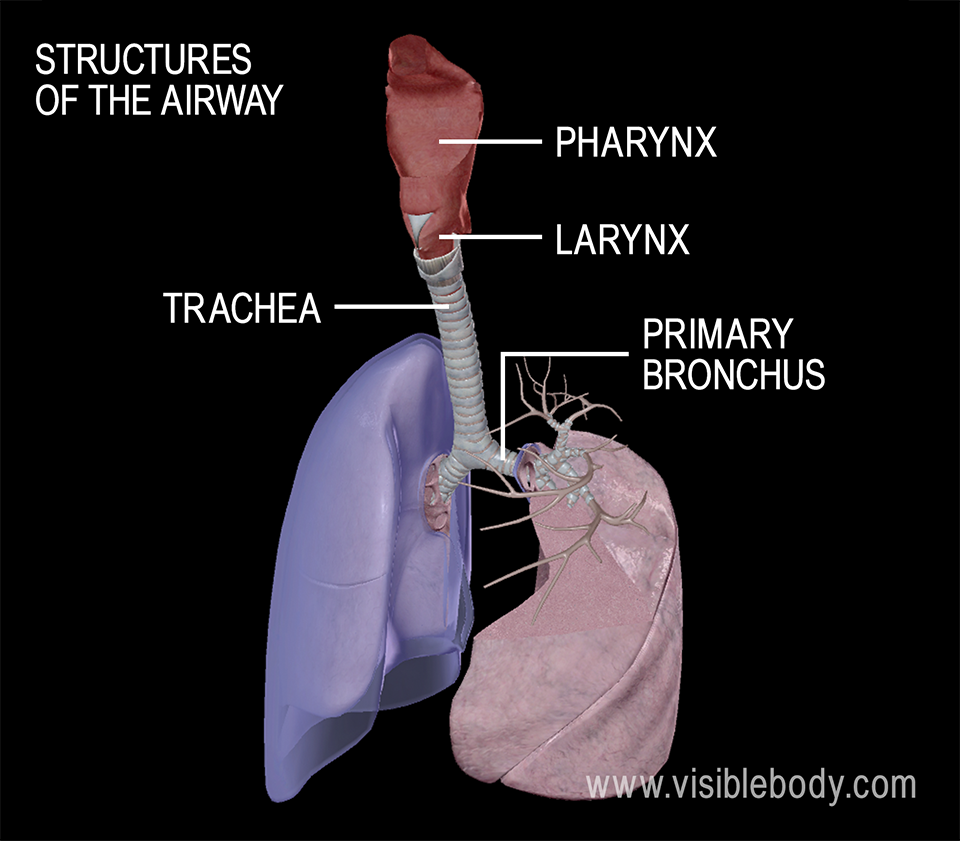
The first thing that emergency medical personnel do when following the ABCDE approach is make sure that a patient’s airway is clear. If it’s blocked, they will attempt to remove the obstruction, whether that means removing a foreign object or placing a tube in the trachea.
The airway refers to the structures of the respiratory system that allow air to flow to and from the lungs: the pharynx, larynx, trachea, bronchi, and bronchioles.
Checking for open airways usually begins with the medical team asking the patient questions. If they’re able to respond normally, it’s a good sign that their airway is clear. Partial obstruction is possible though, and is characterized by changes in the patient’s voice, snoring, gurgling, or noisy and/or effortful breathing. If a patient is unconscious or unresponsive, a head tilt or jaw-thrust maneuver is often used to keep the airway open.
If the airway is obstructed, endotracheal intubation — the placement of a flexible tube in the trachea — is a common method for definitive airway management.
Breathing is often assessed at the same time as the airway. The medical team will evaluate respiration rate, listen for normal breathing sounds, and examine the chest and neck to see if anything is out of place and to ensure that the chest is rising and falling symmetrically.
A "look, listen, and feel" approach is common when checking a patient’s breathing: the person doing the examination will watch for chest movement, place their ear close to the patient’s mouth and nose, and feel for breath on their cheek.
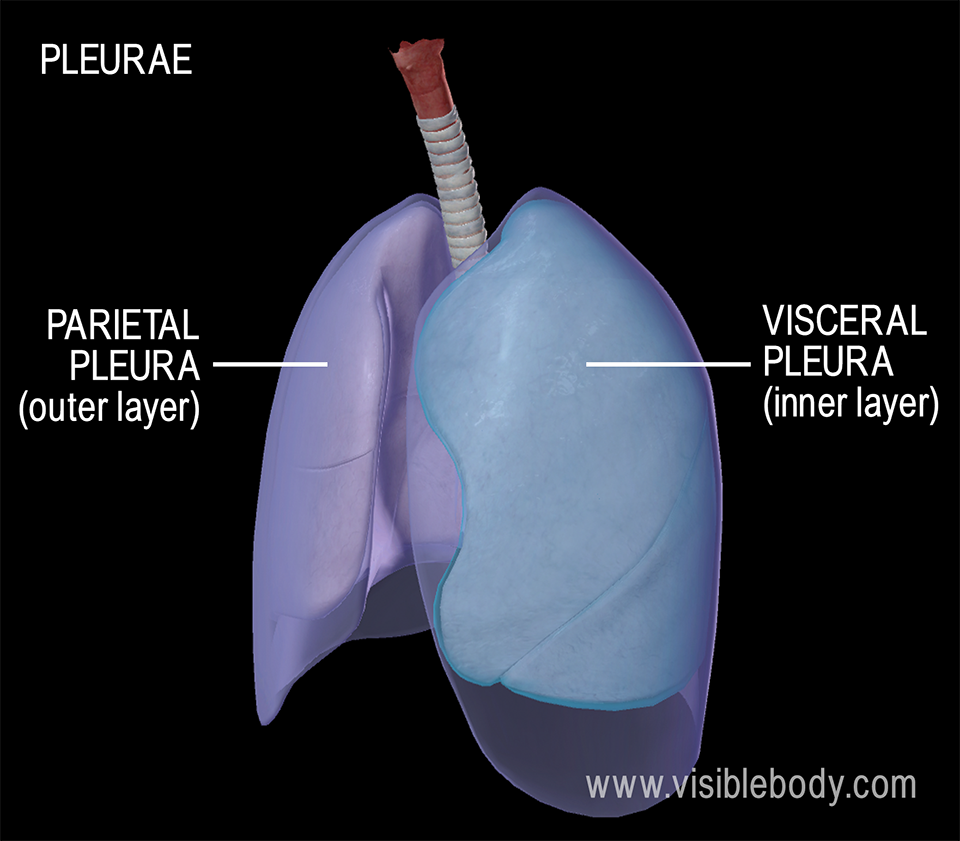
At this stage of trauma assessment, emergency medical professionals know to watch for several life-threatening injuries that affect breathing. Many of these injuries involve the pleurae, membranes that surround the lungs and help to exert pressure on them. This aids the lungs in filling efficiently, so when air or fluid gets between the pleurae, normal breathing is disrupted.
A pneumothorax refers to air that is within the pleural cavity outside the lungs. There are several different kinds, such as tension pneumothorax and open pneumothorax (a "sucking chest wound"), which have different methods for intervention. Symptoms of pneumothorax include sudden chest pain and shortness of breath. A hemothorax is when there is blood in the pleural cavity. Symptoms include chest pain; shortness of breath; rapid, shallow breathing; pale, cool, and clammy skin; and low blood pressure.
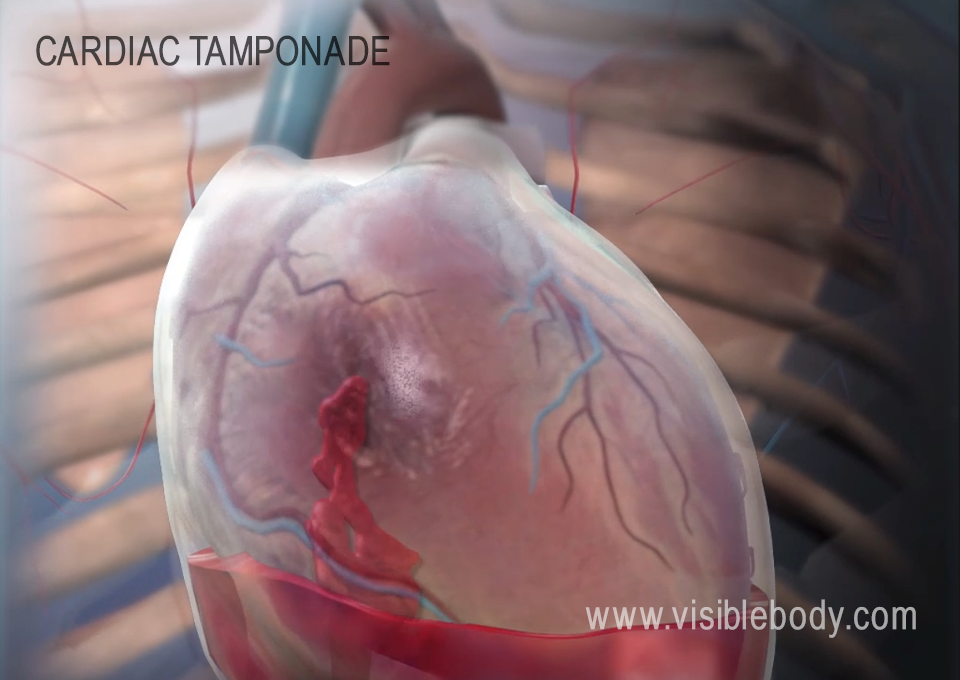
After assessing airways and breathing comes circulation, which means checking the patient’s heart rate and blood pressure, as well as looking for and addressing dangerous conditions such as shock (usually hemorrhagic shock), cardiac tamponade (pressure on the heart caused by fluid buildup in the pericardium), or injury to the aorta.
The pulse would be tested on a patient’s extremities to ensure that blood is flowing properly throughout the body. Another way to assess bloodflow to the extremities is a capillary nail refill test, in which pressure is applied to the nail bed on a patients’ finger or toe until it turns white and the medical professional times how long it takes for normal coloration to return afterwards. Skin color (whether the skin coloration looks normal or is pale/ashy) can also be a clue to circulation.
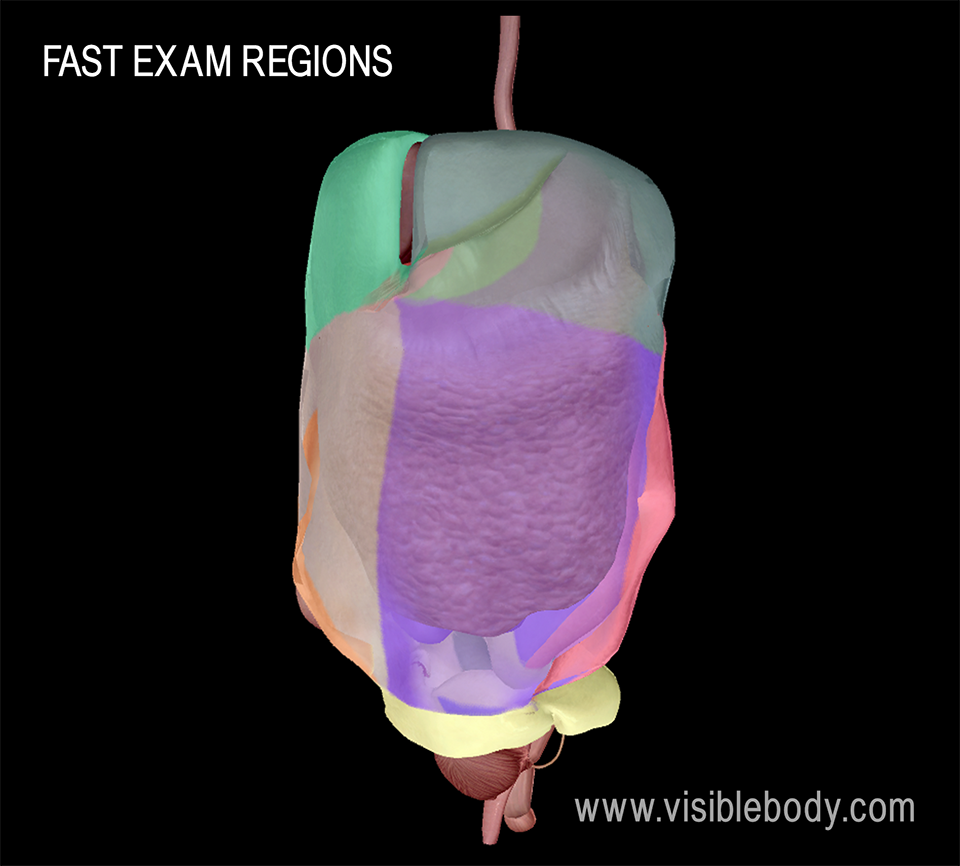
Controlling bleeding and restoring blood volume in cases of significant blood loss are also key components of this step. External hemorrhaging is typically managed in emergency situations with a tourniquet or direct pressure until further treatment for injury is available. Medical professionals will often conduct additional physical exams to look for signs of internal injury, as well as X-Rays of the chest, pelvis, and or extremeties. They might also use special a ultrasound exam called the FAST or E-FAST exam that looks for fluid buildup in the chest and abdomen.
Next comes assessment of neurological function. To evaluate the central nervous system (the brain and spinal cord) for injury, medical teams will assess the patient’s level of consciousness, reflexes such as the size and reaction of the pupils of the eyes, and the patient’s ability to move and feel their extremities.
Impairment to the patient’s ability to move or feel their extremities, weakness, lack of coordination or balance, as well as any numbness or tingling in the hands or feet can be signs of spinal cord injury. In unconscious patients, spinal cord injury can be more difficult to assess. If an injury to the back or neck is suspected, this will have to be taken into consideration while treatment is being provided—that is, keeping airways open and stopping bleeding will need to be done without disturbing the spine, as that could cause further injury.
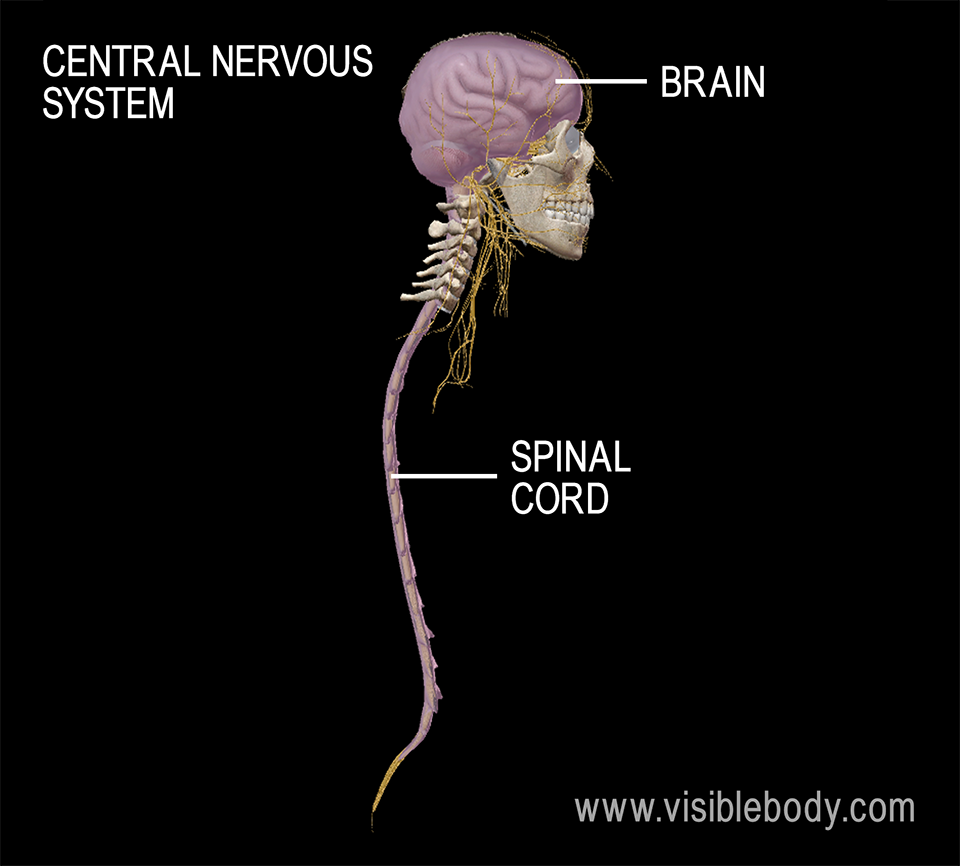
Medical professionals use the Glasgow Coma Scale to check for and rate the severity of traumatic brain injury. The results of the GCS guide clinicians in offering further imaging, such as a CT scan. In cases of traumatic brain injury it is important to avoid further (secondary) injury due to hypoxia (low level of oxygen) or hypoperfusion (not enough bloodflow) to brain tissue.
The "last" part of the ABC(DE) approach to trauma assessment is exposure—that is, removing the patient’s clothing in order to make sure clinicians don’t miss any injuries the patient might have. A full physical exam and medical history is done at this point, as well as any additional necessary X-rays or CT scans. SAMPLE is an acronym many medical professionals use when going over a patient’s medical history:
"Approach to the trauma patient – ABCDE of trauma care" from the International Emergency Medicine Education Project
ACS/ASE medical student guide to initial trauma evaluation
Mayo Clinic articles on diseases and conditions: "Pneumothorax," "Spinal Cord Injury"
Medline Plus Medical Encyclopedia entries: "Capillary nail refill test," "Cardiac tamponade," "CPR (Adult)," "Shock"
NCBI Bookshelf StatPearls article: "Pneumothorax"
When you select "Subscribe" you will start receiving our email newsletter. Use the links at the bottom of any email to manage the type of emails you receive or to unsubscribe. See our privacy policy for additional details.