What Is Polycystic Ovary Syndrome?
Posted on 9/22/23 by Sarah Boudreau
Polycystic ovary syndrome (PCOS) is a set of symptoms stemming from a hormonal imbalance that affects females of reproductive age. Affecting somewhere from 5-15% of females, it’s one of the leading causes of female infertility, and it’s the most common hormonal disorder in females.
In this blog post, we’ll explore PCOS and its causes, diagnosis, and treatment using visuals from the interactive 3D PCOS model and others in Visible Body Suite.
Normal ovarian cycle and PCOS
During the ovarian cycle, follicles containing oocytes mature, the oocyte is released into the uterine tube, and then the empty follicle develops into the corpus luteum. For more information on the ovarian cycle, you can read this whole blog post on the topic!
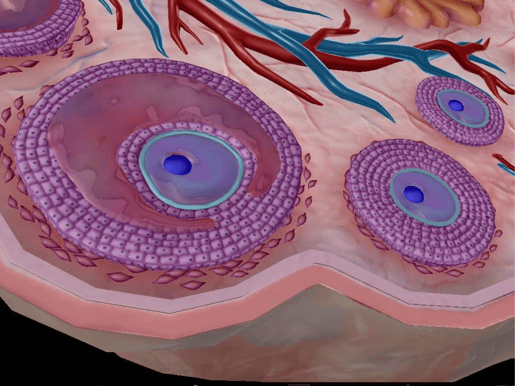
In the ovarian cycle, follicles mature; the primary follicle (right) matures into the secondary follicle (left), which then develops into the vesicular follicle. Image from Visible Body Suite.
A normal ovarian cycle depends on hormones to function. When hormone levels are abnormal, follicles don’t mature fully, which prevents them from releasing oocytes into the uterine tube, a process called ovulation. Without ovulation, immature follicles can accumulate on the ovary, creating bumps that can cause inflammation and irritation of tissues.
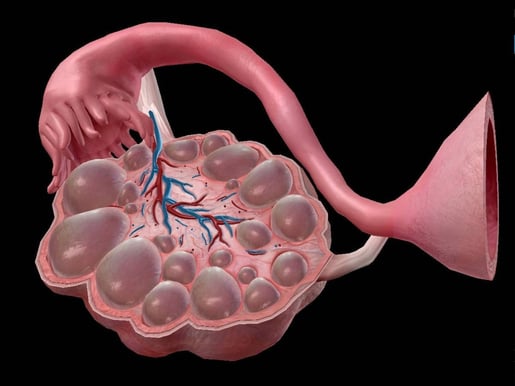
PCOS model in Visible Body Suite.
The process by which the follicle forms the corpus luteum is called luteinization; with PCOS, this part of the ovarian cycle is also disrupted. The corpus luteum typically produces progesterone, but the corpus luteum can’t develop without a mature follicle, so progesterone levels don’t increase.
What’s so special about progesterone? The most important function of this hormone is to prepare the uterus to accept a fertilized egg. Progesterone also regulates menstruation and stimulates glandular development.
When disrupted luteinization leads to a lack of progesterone, the hypothalamus creates gonadotropin hormone-releasing hormone (GnRH), which in turn leads to high levels of luteinizing hormone (LH) and low levels of follicle-stimulating hormone (FSH). Theca cells, which surround the follicle, produce androgens (male sex hormones) in response to the FSH, which can cause symptoms like acne and excess hair growth. .jpg?width=515&height=386&name=screenshot%20-%202023-09-18T115849.893%20(1).jpg)
Hypothalamus highlighted in blue. Image from Visible Body Suite.
What causes PCOS?
The exact cause of PCOS is unknown, but like many other diseases, it’s thought to be a combination of environmental and genetic factors. Researchers have identified some genes that have been tied to PCOS and have estimated about 70% heritability.
Some believe that when genetic predisposition to PCOS meets factors like obesity and insulin resistance, PCOS occurs. Low birth weight, early puberty, and rapid weight gain in infancy are some other risk factors that may contribute to PCOS.
There are several conditions associated with PCOS, including
- Metabolic syndrome
- Obesity
- Depression
- Glucose intolerance
- Type 2 diabetes
Many people with PCOS have insulin resistance, which may be connected to the hormonal imbalances in PCOS. In fact, more than half of people with PCOS develop diabetes by the age of 40.
The hypothalamus, anterior pituitary, and ovaries all need to communicate with each other, but a high level of insulin can disrupt that communication. It’s thought that this can lead to GnRH production from the hypothalamus.
PCOS diagnosis and treatment
Different organizations require slightly different criteria to be diagnosed with PCOS. Using the Rotterdam Criteria, the international criteria for PCOS, you have to have at least two of the following criteria to be diagnosed with PCOS:
- Irregular periods caused by a lack of ovulation
- High levels of male hormones, which can lead to acne and excess face and body hair
- Small cysts on the ovaries
It’s worth mentioning that you can have a higher than average amount of body hair, acne problems, and even polycystic ovaries without having PCOS, which is characterized by its hormonal imbalance.
GIF from Visible Body Suite.
There’s no specific test for PCOS, but doctors may use a pelvic exam, blood tests, and/or a pelvic ultrasound to gather more information.
Diagnosing PCOS can take a while—it can take months to years to receive a diagnosis. This is in part because other conditions have to be ruled out, and diseases like thyroid disease can cause similar signs and symptoms as PCOS. It’s also hard to diagnose in adolescents because many features (like an irregular period) are common in puberty.
PCOS can’t be cured, but it can be treated. Treatment for PCOS includes medication and weight loss, which can reduce symptoms and may increase effectiveness of medications. However, though weight loss is a treatment for PCOS, the hormonal imbalances associated with PCOS can also make it more difficult to lose weight.
There are many different medications prescribed to people with PCOS, including birth control to regulate hormones or medications to help with ovulation, like Clomiphene.
Conclusion
PCOS is a group of symptoms that result from a hormonal imbalance. This imbalance means that the ovary’s follicles don’t mature properly, leading to a lack of ovulation and a buildup of follicles. This can result in cysts on the ovaries. PCOS is connected to several other diseases, such as type 2 diabetes, and though it can’t be cured, it can be treated.
Want to learn more about the ovaries? Check out these blog posts!
- The Ovarian Cycle: A Guide
- 5 Facts About the Ovaries and Ovarian Cancer
- Endometriosis: A Common but Misunderstood Disorder
Visible Body Suite and Courseware users can access free, interactive study content about the male and female reproductive systems—check out our free libraries of premade Flashcard Decks and Tours!
Be sure to subscribe to the Visible Body Blog for more anatomy awesomeness!
Are you an instructor? We have award-winning 3D products and resources for your anatomy and physiology course! Learn more here.



