The Ovarian Cycle: A Guide
Posted on 9/15/23 by Sarah Boudreau
Without the ovarian cycle, you wouldn’t be reading this blog post right now. In fact, I wouldn’t be writing it either! The ovarian cycle is a core part of human reproduction; during the ovarian cycle, follicles in the ovaries mature and release one oocyte per cycle into the uterine tubes, where they can be fertilized and can eventually develop into a fetus.
Today on the Visible Body Blog, we’ll walk through the anatomy and physiology of the ovarian cycle using visuals from Visible Body Suite, including the new, interactive ovarian cycle model.
GIF from Visible Body Suite.
What’s the difference between the menstrual cycle and the ovarian cycle?
The two cycles happen at the same time and influence each other, and they both prepare the body for pregnancy. Simply put, the ovarian cycle is concerned with the ovary and the release of oocytes, and the menstrual cycle is concerned with the uterine lining.
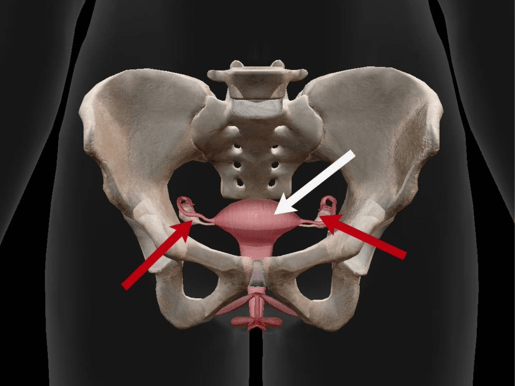
Red arrows point to the ovaries and the white arrow points to the uterus. Image from Visible Body Suite.
Ovaries creates oocytes, which are female gametes. They also produce progesterone and estrogens. The uterus, on the other hand, is where a zygote (a fertilized oocyte) implants and develops—another term for uterus is womb.
Since we’re focusing on the ovarian cycle today, we’ll be taking a closer look at the ovary.
The ovarian cycle
The ovarian cycle occurs in three phases:
- The follicular phase, where the follicles mature
- Ovulation, where the oocyte is released into the uterine tube
- The luteal phase, where the corpus luteum is formed
Let’s explore these phases by looking at the anatomy of the ovary.
Oocytes and primordial follicles
We can’t talk about follicles without first talking about oocytes!
Oocytes first form during fetal development when stem cells undergo mitosis, creating primary oocytes which then begin meiosis. Until puberty, these primary oocytes remain in the prophase stage of meiosis I.
During female puberty, the primary oocytes form primordial follicles, which develop into primary follicles that contain primary oocytes.
Some primary oocytes complete meiosis I to become secondary oocytes, which are 23 chromosome cells that begin but do not complete meiosis II. If the secondary oocyte is fertilized, it completes meiosis and can develop into a zygote.
Primordial, primary, and secondary follicles
Primordial follicles are home to primary oocytes. The primordial follicle is stimulated by follicle stimulating hormone (FSH), developing into a primary follicle. During the follicular phase, one primary follicle develops into a secondary follicle, which is larger. 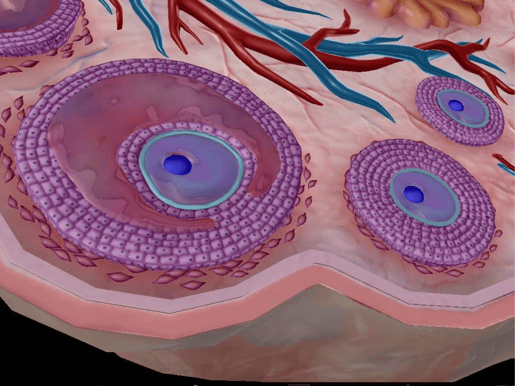
Secondary follicle (left) and primary follicle (right). Image from Visible Body Suite.
Vesicular follicle
A few days before ovulation, the secondary follicle develops into a vesicular follicle. Inside a vesicular follicle, there is a cavity called the antrum that is filled with follicular fluid that contains hormones, enzymes, electrolytes, and anticoagulants. The antrum surrounds the secondary oocyte.
During ovulation, the follicle ruptures and releases the secondary oocyte into one of the uterine tubes, also called the Fallopian tubes.
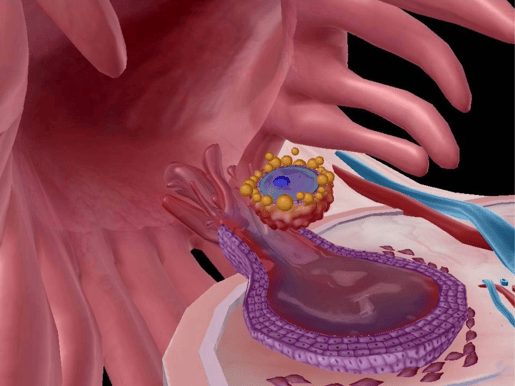
The oocyte enters the uterine tube. Image from Visible Body Suite.
Around the follicle
Each follicle is surrounded by layers of granulosa cells, which support the oocyte and help produce estrogen and progesterone. After menstruation but before ovulation, follicle-stimulating hormone from the anterior pituitary stimulates the granulosa cells to convert androgens to estrogen. That increase of estrogen triggers the anterior pituitary to release luteinizing hormone (LH), which causes a follicle to rupture and release an oocyte.
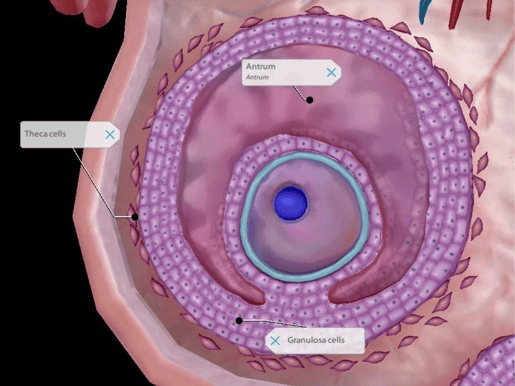
Image from Visible Body Suite.
After ovulation, granulosa cells and theca cells become part of the corpus luteum—more on that soon! Theca cells surround the follicles, and they secrete androgens that the granulosa cells can turn into estrogen.
The zona pellucida forms as follicles develop from primary to secondary. It’s a layer of glycoprotein between the oocyte and granulosa cells that helps ensure the health of the follicles and oocytes as they develop.
Corpus luteum
The corpus luteum develops after ovulation and is what’s left of the follicle that releases the oocyte. It produces estrogen and a lot of progesterone. If the egg becomes fertilized, the corpus luteum will release progesterone for about twelve weeks. Then, the placenta creates the progesterone, and the corpus luteum is broken down. If the oocyte isn’t fertilized, the breakdown process, called luteolysis, begins about ten days after ovulation. After luteolysis, fibroblasts create the corpus albicans, a scar-like structure. .jpg?width=515&height=386&name=screenshot%20-%202023-09-07T183835.507%20(1).jpg)
Image from Visible Body Suite.
Conclusion
The ovaries create oocytes. During the ovarian cycle, follicles in the ovaries mature and rupture. They release an oocyte into the uterine tube in a process called ovulation. After ovulation, the remainder of the follicle breaks down into the corpus luteum, which then forms the corpus albincans. Then the cycle starts all over again!
Want to learn more about the female reproductive system? Check out these blog posts!
- Anatomy and Physiology: Internal Female Reproductive Anatomy
- 5 Facts About the Ovaries and Ovarian Cancer
- Beyond Just XX or XY: The Complexities of Biological Sex
- Endometriosis: A Common but Misunderstood Disorder
Visible Body Suite and Courseware users can access free, interactive study content about the male and female reproductive systems—check out our free libraries of premade Flashcard Decks and Tours!
Be sure to subscribe to the Visible Body Blog for more anatomy awesomeness!
Are you an instructor? We have award-winning 3D products and resources for your anatomy and physiology course! Learn more here.



