Physiology & Pathology: Four Common Cardiovascular Conditions
Posted on 11/14/19 by Laura Snider
A properly-functioning heart is really important when it comes to staying alive. This muscular organ works 24/7 to pump blood out to the furthest reaches of your body, providing your organs and tissues with oxygen and nutrients. When the heart has trouble performing this key function, the results can be catastrophic.
We’ve talked about atherosclerosis, heart disease, and stroke on the Visible Body blog before, but with the release of Physiology and Pathology, we can now look at heart conditions in even more depth and detail!
Here are four common cardiovascular conditions, their effects on the body, risk factors that contribute to them, and ways doctors treat them.
1. Coronary artery disease
Coronary artery disease (CAD) is not only the most common type of heart disease—it’s also the leading cause of death in the United States in both men and women (yikes!).
Needless to say, coronary artery disease is serious business. That’s because it has pretty scary complications, most notably heart attacks.
So what happens when someone has coronary artery disease? As the name indicates, this type of cardiovascular disease affects the coronary arteries—that is, the arteries that supply the muscles of the heart. The buildup of plaque inside the coronary arteries causes them to narrow. It’s basically a special (or rather, an especially nasty) instance of atherosclerosis.
When the coronary arteries are obstructed by plaque, blood flow to the muscles of the heart decreases. This is a type of ischemia, which is a general term for when tissues or organs are deprived of the oxygen and nutrients blood brings.
Now, you can probably imagine how bad it would be if those muscles stopped working, and that’s pretty much what happens if they can’t get the blood and nutrients they need. If a blood clot blocks off blood supply to the muscles of the heart, either completely or partially, a myocardial infarction (a heart attack) occurs.
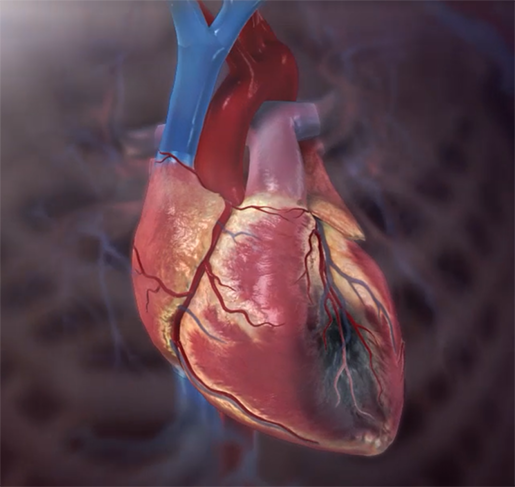 A heart attack in progress. Animation screenshot from Physiology & Pathology.
A heart attack in progress. Animation screenshot from Physiology & Pathology.
According to the Mayo Clinic, the classic presentation of a heart attack is as follows:
- Pressure, tightness, pain, or a squeezing or aching sensation in your chest or arms that may spread to your neck, jaw, or back
- Nausea, indigestion, heartburn, or abdominal pain
- Shortness of breath
- Cold sweat
- Fatigue
- Lightheadedness or sudden dizziness
However, it’s important to remember that heart attacks don’t present the same way in everyone. Oftentimes, men and women report different symptoms. If you believe you’re having a heart attack, it’s important to seek out medical help right away.
Fortunately, there’s a lot people can do to decrease their risk of coronary artery disease (and having a heart attack). Not smoking cigarettes is a big one, and so is maintaining a healthy diet and making sure to exercise regularly. Keeping an eye on one’s cholesterol level and blood pressure and working with a doctor to keep those in a healthy range is also a good idea.
2. Hypertension
Hypertension is pretty much exactly what it sounds like: high pressure. In this case, high blood pressure. When you get your blood pressure measured, two numbers are usually recorded. The first of these numbers is systolic pressure, which measures (in mm Hg) the pressure your blood exerts on the walls of your arteries during systole, the phase of the cardiac cycle when the ventricles contract and blood is pushed out of the heart. The second number is diastolic pressure, which measures the pressure exerted by the blood on the walls of your arteries during diastole, the phase of the cardiac cycle when the ventricles are not contracting and the atria fill with blood.
According to the American Heart Association, the normal range for blood pressure is a systolic pressure of 120 mm Hg or less and a diastolic pressure of 80 or less. If the systolic pressure is 120-129 mm Hg but the diastolic pressure is still 80 or less, the blood pressure is considered to be elevated. The threshold for hypertension (stage 1) is a blood pressure of 130-139 / 80-89 mm Hg.
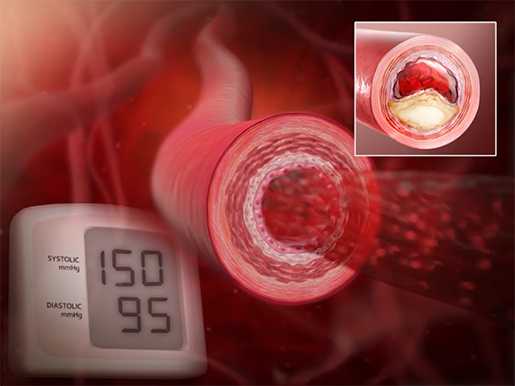 Animation screenshot from Physiology & Pathology.
Animation screenshot from Physiology & Pathology.
Hypertension can develop either with or without an underlying condition (kidney problems, obstructive sleep apnea, diabetes, thyroid problems). Certain medications can also cause high blood pressure. Since it generally develops over time, it may not surprise you to know that the risk of hypertension increases with age. Smoking, heavy drinking, low physical activity, a high-sodium diet, and high chronic stress levels can also increase your risk of developing high blood pressure.
So what’s so dangerous about high blood pressure? Over time, high blood pressure can damage your blood vessels and even your internal organs. If a blood vessel becomes sufficiently weak, a bulge called an aneurysm can form. Depending on the location of the aneurysm, the results of it bursting could be fatal. Heart failure can also result from hypertension—essentially, the heart has to work extra hard to overcome the higher pressure and its muscles thicken (hypertrophy), making blood-pumping even more difficult. Atherosclerosis (with carries with it the risk of heart attack and stroke) is another issue that can potentially be caused by hypertension.
Hypertension can be managed with lifestyle changes (such as a low-sodium, heart-healthy diet, maintaining a healthy weight, and exercising regularly) and medication.
3. Mitral valve prolapse (the real MVP)
Valves in the circulatory system perform a vital public service: preventing the backflow of blood into veins and heart chambers.
 The heart valves opening and closing during the cardiac cycle.
The heart valves opening and closing during the cardiac cycle.
Video footage from Physiology & Pathology.
Around 2% of people have a condition called mitral valve prolapse (MVP), in which the mitral valve—the bicuspid valve that separates the left atrium from the left ventricle—doesn’t close properly during ventricular contraction. This means that when the ventricles squeeze blood out of the heart, part of one or both of the mitral valve’s leaflets prolapses (bulge) back into the left atrium. Sometimes this also allows a little bit of blood to flow back into the left atrium.
 Mitral valve prolapse and blood flowing back into the left atrium.
Mitral valve prolapse and blood flowing back into the left atrium.
Video footage from Physiology & Pathology.
Mitral valve prolapse is typically caused by overly-stretchy valve leaflets. Also, here’s a fun(?) fact: mitral valve prolapse can run in families!
Sometimes, if heart function gets worse and/or the left ventricle becomes enlarged, the mitral valve may need to be repaired or replaced. Mitral valve prolapse can also lead to arrhythmias (irregular heartbeats) in severe cases. If a lot of blood leaks back into the left atrium, blood clots can form. This could cause a stroke or a heart attack.
Most of the time, though, mitral valve prolapse doesn’t require treatment. It’s just kind of there and can be uncomfortable but rarely becomes a serious problem. The American Heart Association lists the common symptoms as “bursts of rapid heartbeat (palpitations), chest discomfort and fatigue.”
4. Arrhythmias
Typically, the heart beats at 60-100 bpm (resting HR varies depending on a number of factors, but it’s usually within this range). The heart beats faster during exercise, but slows down when you’re just hanging out.
If the conduction system of the heart isn’t working properly, irregular heart rhythms (arrhythmias) can result.
 The heart conduction system in action. Video footage from Physiology & Pathology.
The heart conduction system in action. Video footage from Physiology & Pathology.
Arrhythmias are often classified according to the direction of heartbeat abnormality (fast vs. slow) and where in the heart the problem is occurring (atria, ventricles, and so on). A resting heart rate of over 100 bpm is known as tachycardia, and a heart rate below 60 bpm is called bradycardia. Both types of abnormalities reduce stroke volume and can lower cardiac output.
Arrhythmias can also be described based on what type of abnormality is involved. Sinus arrhythmias occur when the sinoatrial (SA) node has an abnormal rate of firing. Re-entrant circuit arrhythmias occur when the electrical impulses in the heart travel in circular pathways, causing repeated stimulation. Heart block arrhythmias occur when the electrical signals in the conduction system are delayed or blocked. Re-entrant circuit and heart block arrhythmias can cause the atria and ventricles to contract independently, which causes cardiac output to decrease.
There are many factors that influence whether a person develops an arrhythmia. Having other heart problems such as coronary artery disease, hypertension, congenital heart defects, or past heart attacks can definitely increase the risk of developing an arrhythmia. Certain prescription drugs, thyroid problems, electrolyte imbalance diabetes, and obstructive sleep apnea can also play a role. So can lifestyle factors like smoking, alcohol use, caffeine use, and stress.
Common symptoms of arrhythmias include chest pain, weakness, and hypotension. If your heart feels like it’s a DJ trying to lay down some funky beats (in other words, if your heart’s racing, beating too slowly, or fluttering, or if you are experiencing any of the symptoms listed on this page), it’s a good idea to see a doctor. Ultimately, arrhythmias can be extremely dangerous—heart failure and stroke are both potential complications.
Arrhythmias can be treated with medication, surgical procedures, or implanted devices (pacemakers, for example). Lifestyle changes such as eating a heart-healthy diet, exercising regularly, stopping smoking, and keeping blood pressure and cholesterol levels in check are also often recommended alongside these treatments.
The main takeaways here are as follows.
- Heart health is important! Don’t neglect it.
- In most cases, there’s a lot you can do to help your heart live its best life, such as maintaining good nutrition, making sure to exercise, and working with your doctor to make sure your heart’s functioning properly.
Be sure to subscribe to the Visible Body Blog for more anatomy awesomeness!
Are you an instructor? We have award-winning 3D products and resources for your anatomy and physiology course! Learn more here.



