The Precious Pancreas: Insulin, Glucagon, and Digestive Juices
Posted on 10/10/19 by Adelaide Elkin
Located behind the stomach and at the back of the abdomen is the six-inch-long, tadpole-shaped pancreas. From head to tail, the pancreas extends across the abdomen. The head (the wide part of the pancreas) is based where the stomach meets the duodenum (the first part of the small intestine).
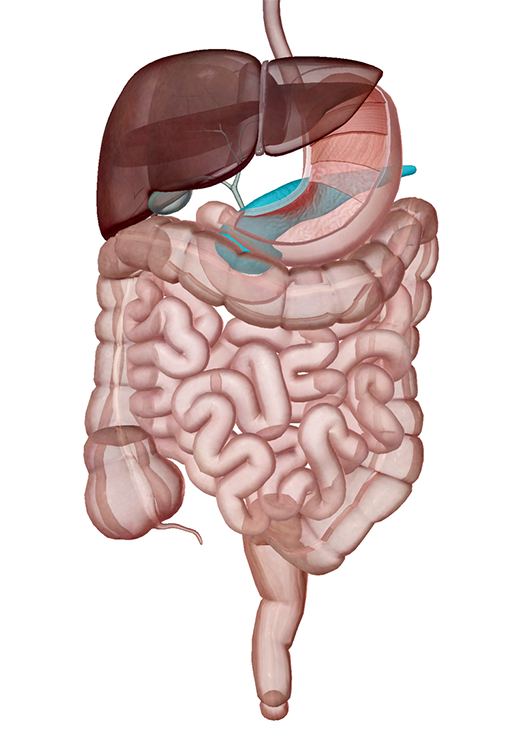 The pancreas in context. Image from Human Anatomy Atlas.
The pancreas in context. Image from Human Anatomy Atlas.
The pancreas is an accessory digestive organ made of small glandular clusters of epithelial cells. It’s crucial for converting food to fuel for body cells and contains both endocrine and exocrine gland cells.
Endocrine and Exocrine Functions of the Pancreas
The exocrine cells of the pancreas produce enzymes that combine with electrolytes and water to become part of a digestive fluid called pancreatic juice. It is carried by a network of pancreatic ducts to the small intestine. The juice promotes digestion as it helps break down carbs, fats, and proteins. About 1200-1500 mL of pancreatic juice is produced daily!
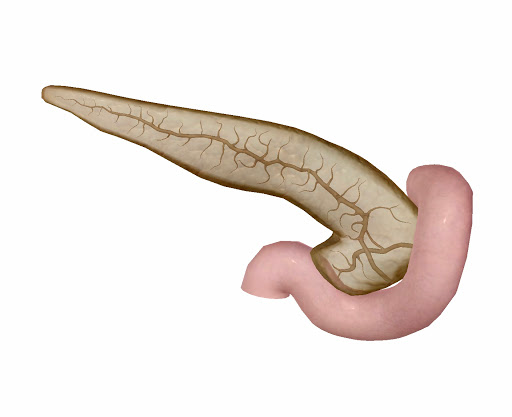 The pancreas (posterior view), its ducts, and the duodenum. Image from Visible Body Suite.
The pancreas (posterior view), its ducts, and the duodenum. Image from Visible Body Suite.
The pancreas also contains around a million pancreatic islets (or islets of Langerhans), which are hormone-producing cell clusters. The islets contain two major populations of hormone producing cells: the glucagon-synthesizing alpha cells and the insulin-synthesizing beta cells. These cells secrete glucagon or insulin during the fasting and full states and can sense when the body needs and doesn’t need food.
%20(1).jpg?width=515&height=386&name=screenshot%20(5)%20(1).jpg)
Image from Visible Body Suite.
Insulin and Glucagon
Insulin and glucagon are the hormone pair that regulates glucose levels.
Insulin:
Insulin is secreted when blood glucose is high. It signals cells to take up glucose and convert it into energy or other substances like glycogen or fats, while also promoting protein synthesis and fat storage.
Its effect is most prominent after eating. Its prime job is to lower blood glucose levels (while also influencing fat and protein metabolism) and it does so in three ways:
- It enhances membrane transport of glucose into body cells, and promotes the storage of fat in fat cells and glycogen in muscle cells
- It prevents the breakdown of glycogen to glucose (in muscle)
- It prevents the conversion of amino acids to glucose
The beta cells reduce insulin secretion when the blood levels of glucose and other nutrients drop as the body absorbs them.
Glucagon:
A decrease in glucose levels (and rising amino acid levels) activate the alpha cells to secrete glucagon. It is an extremely powerful hormone—one molecule can cause the release of 100 million glucose molecules into the blood!
Glucagon’s prime focus is the liver where it promotes the following:
- Breakdown of glycogen into glucose
- Synthesis of glucose from lactic acid and noncarbohydrate molecules
- Release of glucose to the blood from liver cells, causing blood glucose levels to rise
The alpha cells reduce glucagon secretion when blood glucose and insulin levels rise.
Pancreas Pathologies
The pancreas can be quite problematic. When insulin levels are thrown off balance, it can result in a common condition called diabetes mellitus (DM).
There are two types of the condition that occur depending on whether there is hyposecretion or hypoactivity of insulin. Type one diabetes occurs when the body does not make enough insulin. Type two diabetes occurs when cells become resistant to insulin, which can eventually lead to lower insulin levels. In both cases, blood sugar remains high. When blood glucose levels increase, hyperglycemic hormones (i.e. glucagon) are not released, and when glucose levels become excessive, the body’s response isn’t so pretty.
Nausea is often the first symptom. This activates a fight or flight response causing the body to act as though it were in the fasting state, then producing even more glucose. The body has no idea what to do with all that glucose and eventually resorts to expelling excess glucose through urine. Prolonged high blood sugar can also damage the retina, leading to conditions such as diabetic retinopathy.
When glucose is unable to enter body cells, it causes high fatty acid levels in the blood. This is a condition known as lipidemia. When the fatty acid ketones or ketone bodies (acidic organic compounds) amass in the blood, the blood pH declines, causing the ketone bodies to exit through (once again) urine, because apparently that’s the body’s way of avoiding its problems. This is a condition called ketoacidosis, which is life threatening if severe.
Another common condition, pancreatitis, is inflammation of the pancreas caused by a buildup of the enzymatic juice that causes the organ to essentially digest itself (yikes). The condition shows up in two forms: either chronic or acute. Acute pancreatitis is sudden and usually the result of alcohol ingestion, gallstones, a reaction to medication, infections, or trauma. If left untreated, it can be life-threatening, but if properly cared for, full recovery is likely.
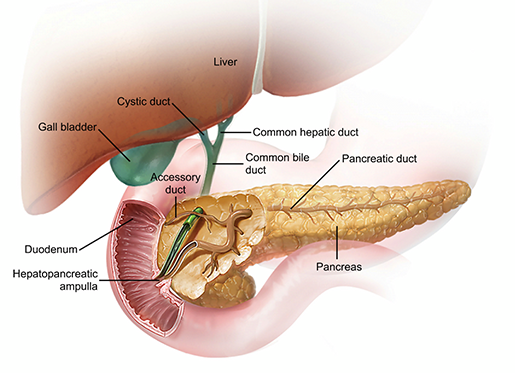 The pancreas, liver, gall bladder, and ducts. Image from Visible Body Suite.
The pancreas, liver, gall bladder, and ducts. Image from Visible Body Suite.
Chronic pancreatitis occurs when the health of the pancreas progressively worsens over time and is commonly the result of alcohol abuse, but can also be hereditary or the result of cystic fibrosis.
Some people are born with a condition called pancreas divisum: when two parts of the pancreas (the ventral duct and the dorsal duct) do not fuse together, typically during development in the womb. Symptoms don’t usually come with pancreas divisum, although in rare cases some may experience nausea, vomiting, abdominal pain, or acute/chronic pancreatitis. Treatment for those who don’t experience any symptoms is not necessary, but a surgical procedure may be needed for those with symptoms.
Pancreatic cancer is perhaps the worst pancreas pathology of all. The disease arises when a malignant tumor forms in any part of the pancreas.
Pancreatic adenocarcinoma is the most common form of pancreatic cancer and occurs in the exocrine tissue. This type of pancreatic cancer is the result of abnormal cell growth lining the walls of the pancreatic duct.
Uncommon as they are, endocrine tumors begin in the pancreatic islet cells. This can cause additional problems, since these are hormone-producing cells that can cause the tumor itself to produce hormones. The endocrine tumors that produce excessive amounts of hormones are called neuroendocrine tumors (as the endocrine gland does not lose functionality).
Also derived from the pancreatic islet cells, insulinomas produce excessive amounts of insulin, causing low blood sugar. These tumors are normally benign and cause minor symptoms such as dizziness, fatigue, weakness, or hunger. The tumors normally require surgical removal but are relatively mild compared to other pancreatic tumors.
Treatment for pancreatic cancer heavily depends on the stage of the disease, general health of the patient, and the specific characteristics of the cancer. Patients typically have a variety of options for treatment such as chemotherapy, radiation therapy, surgery, and palliative care.
So, try to keep your pancreas happy and healthy by not ingesting anything potentially harmful. Instead, next time you get hungry, thank your pancreas and those precious hormones for giving you a valid excuse to eat! From hunger to fullness, your pancreas tells you when to stuff yourself silly, or maybe take it easy on the nachos.
Be sure to subscribe to the Visible Body Blog for more anatomy awesomeness!
Are you an instructor? We have award-winning 3D products and resources for your anatomy and physiology course! Learn more here.
Additional Sources:




