[Non-COVID] Medical News Roundup 2021
Posted on 12/10/21 by Sarah Boudreau
2021 was a huge year for health news here in the United States as COVID vaccines were rolled out and we had to learn several fraternities’ worth of Greek letters as mutations kept popping up.
In all the pandemic hubbub, you might have missed out on other medical news, so we are going to recap five of the year’s notable medical news stories.
1. Gene Editing Restores Some Vision for People with Genetic Disorder
Researchers at Oregon Health & Science University are collaborating with the pharmaceutical companies Editas Medicine and Allergan to conduct a landmark clinical trial for people with Leber’s congenital amaurosis.
Leber’s congenital amaurosis (LCA) is a leading cause of blindness in children, and there is no treatment currently available. LCA causes a mutation in the gene CEP 290 and disables photoreceptors in the retina, which detects light and color. LCA starts in infancy and can get slowly worse over time; people with LCA usually become legally blind.
 GIF from Human Anatomy Atlas.
GIF from Human Anatomy Atlas.
The trial uses the gene editing technology CRISPR. Using the CRISPR-Cas9 technique, scientists create RNA that binds itself to a specific sequence of DNA and to the Cas9 enzyme. The RNA shows the Cas9 where to cut the cell’s DNA. Then, scientists can manipulate the cell’s DNA repair mechanisms to make changes to the genetic material.
CRISPR-Cas9 is the best genome editing method we’ve got: it’s faster, cheaper, and more accurate than other CRISPR methods.
Previous similar clinical trials have tried to remove cells from the body, edit them, and re-insert them, but this trial uses CRISPR directly on the eye to delete the mutation in CEP 290.
Patients received different doses, and some have reported vision improvements. Many are now able to determine shapes and colors. They are not expected to develop normal vision, but every improvement makes a big difference to the patients.
There still needs to be more research and more trials to see how safe and effective this treatment is, but this is a promising start.
2. Sleep Bootcamp Helps Older Adults
If you’re an older adult with insomnia, training yourself to break bad sleep habits can help prevent depression.
According to the CDC, older adults have an increased risk for depression. 80% of older adults have at least one chronic health condition, which also increases risk for depression. Older adults are also more likely to spend time alone, and social isolation and loneliness are associated with higher depression rates.
You know what else is a major risk factor for depression? Insomnia! Approximately 10-30% of the population has insomnia.
 Photo from Shutterstock.
Photo from Shutterstock.
Researchers have found a way to help this through cognitive behavioral therapy—and not medication. A medication-free approach is desirable because older adults might already be taking medications, and this means that there’s no risk of drug interactions.
Cognitive behavioral therapy (CBT) is one of the leading forms of psychological treatment and is one of the most tried and true forms of therapy. CBT involves re-working thinking patterns. During CBT, you work with a mental health professional to recognize when your thoughts cause problems and use problem solving skills to rework your thoughts and change patterns of behavior.
The trial included adults over 60 years of age who had insomnia but not depression. The control group received eight weeks of basic sleep education while the other group got eight weeks of CBT-I, a form of CBT that focuses on insomnia. They worked with trained therapists in a group setting.
In the trial, those who received CBT for insomnia were two times less likely to develop depression. After three years, about a third of the CBT-I people were still insomnia-free, but the sleep education people did not fare as well.
3. First Person Cured of Type 1 Diabetes… Maybe
An Ohio man may be the first person to be cured of type 1 diabetes.
While type 2 diabetes occurs when cells develop a resistance to insulin, type 1 diabetes occurs when the pancreas produces little to no insulin. Insulin is a hormone that allows sugar to enter cells. In type 1 diabetes, the immune system destroys the pancreas’s insulin-producing islet cells. Diabetes is a leading cause of blindness and kidney failure. It also weakens the immune system. Insulin is expensive and pancreas or islet cell transplant is not feasible for most people. There is no proven cure for type 1 diabetes.
The pancreas, liver, gallbladder, and ducts. Image from Anatomy & Physiology.
The pharmaceutical company Vertex figured out how to consistently turn stem cells into islet cells. Those islet cells were implanted into people with severe type 1 diabetes. The participants take immunosuppressive drugs to keep their bodies from rejecting these new cells.
The study is still in progress and has 17 people with severe type 1 diabetes.
The New York Times reported that one participant received “cure-like results” 90 days after the islet cell transplantation. His body seems to be able to maintain its blood sugar levels without any catastrophic crashes.
However, this doesn’t mean there is a cure for type 1 diabetes—some have criticized The New York Times for being sensationalist, since they reported on this so soon. This is a five-year study, and we are only at the tip of the iceberg.
4. Cancer Deaths on the Decline
I once heard someone say that the reason we pay more attention to bad news is that bad news happens all at once, but good news is gradual. I’ve got some good news that might not look as flashy as the bad, but it’s still worth your attention: cancer death rates in the United States are declining.
A report from the American Cancer Society, Centers for Disease Control and Prevention, the National Cancer Institute, and the North American Association of Central Cancer Registries measured cancer deaths from 2014-2018, the most recent period for which they have data.
They found some exciting stuff:
- Decreased death rates for 11 out of the 19 most common cancers among men
- Decreased death rates among children
- Declining death rates for all racial and ethnic groups
A large factor in this decrease is that melanoma and lung cancer fatalities have decreased.
But why is that?
Firstly, treatment for these cancers has improved. More and more people are also getting screened, which means that doctors can catch the cancer while it’s in early—and thus more treatable—stages.
For lung cancers, another reason is the decline of smoking. In the last year of the survey, 2018, smoking reached an all-time low. Smoking has decreased by two thirds in the past 50 years, but it’s still the leading cause of preventable death in the United States.
Overall cancer deaths may have decreased, but death rates for certain cancers have increased, like colorectal and breast cancers. To keep your risk for cancer low, doctors recommend a healthy lifestyle: diet and exercise, reduced alcohol consumption, no smoking. Certain vaccinations like the ones for human papillomavirus and hepatitis B can further reduce risk.
5. Surgeons Perform First Successful Trachea Transplant
On January 13th, doctors completed the first successful tracheal transplant.
The patient had trachea damage from intubation for a severe asthma attack six years ago. After several surgeries, she had to have a tracheostomy, where an opening was created in the front of her neck.
Historically, the biggest barrier to tracheal transplant is ensuring blood flow to the new trachea. For many years, doctors thought that the trachea needed many blood vessels to get its supply of blood.
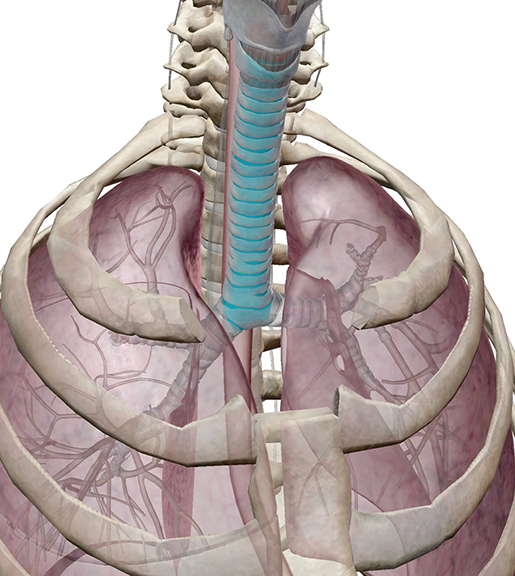 Image from Human Anatomy Atlas.
Image from Human Anatomy Atlas.
Instead of focusing on transplants, they shifted to trying to figure out how to replace the trachea. Italian surgeon Paolo Macchiarini made headlines when he claimed that he used polymers to create scaffolding that used a patient’s cells to create a trachea. Macchiarini made headlines again when he was accused of research misconduct and was discredited. In 2019, he was sentenced to 16 months in prison in Italy for forging documents and abuse of power.
At Mount Sinai Hospital in New York, Dr. Eric Genden found that a tracheal transplant could be possible after all: the trachea could receive adequate blood supply with only a few blood vessels.
Surgeons took eighteen hours to remove the trachea from a donor, transplant it into the patient, and connect veins and arteries to the newly-transplanted organ.
The patient’s body quickly got to work incorporating its cells and replacing the donor’s cilia, the small, hairlike projections that trap and move particles in the trachea.
It will take more time to make sure that the surgery was fully successful, but doctors find it promising. The surgery launched Mount Sinai’s new Tracheal Transplant Program.
Conclusion
2021 was certainly an exciting year for medical discoveries and innovations. We here at Visible Body hope you have a great holiday season and a happy new year, and we look forward to another year of advancements in medicine.
Be sure to subscribe to the Visible Body Blog for more anatomy awesomeness!
Are you an instructor? We have award-winning 3D products and resources for your anatomy and physiology course! Learn more here.



