Exploring Skeletal and Muscular System Pathologies with Physiology & Pathology
Posted on 12/19/19 by Laura Snider
Ready to use Visible Body’s new app, Physiology & Pathology, to explore some more pathologies? Today, we’re going to focus on pathologies of the skeletal and muscular systems.
The skeleton and the muscles that attach to it are what give your body structure and allow it to move but, just like your internal organs, your bones and muscles can be affected by a wide range of injuries and diseases.
1. Fractures, Sprains, and Strains
Many, if not most, people have probably experienced one of these types of injuries—maybe you fell out of a tree and broke your arm as a kid, took a wrong step and sprained your ankle, or pulled one of your hamstring muscles during a workout. Or maybe you’re one of the lucky few who hasn’t suffered from a fracture, strain, or sprain. Either way, they’re still among the most commonly reported sports injuries (and “being a clumsy person” injuries, as I can personally attest on the sprained ankle front).
Let’s start with fractures. When a bone is broken, your body springs into action to fix it. First, a hematoma forms at the fracture site as blood clots. Then, special cells called osteoclasts clean out dead bone tissues and fibroblasts build a callus around the fracture.
 Osteoclasts: the cleanup crew arrives!
Osteoclasts: the cleanup crew arrives!
Animation screenshot from Physiology & Pathology.
This callus will eventually be turned into bone by osteoblasts (cells that generate new bone), but this can take a while.
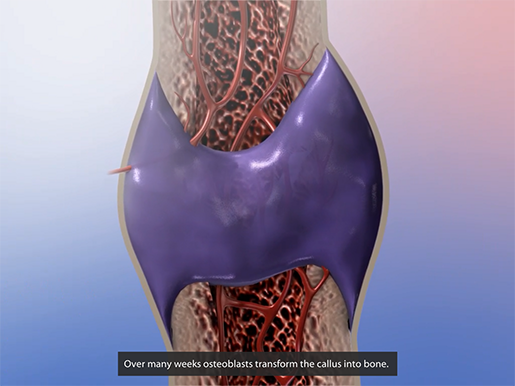 Callus formed by fibroblasts, to be turned into bone by osteoblasts.
Callus formed by fibroblasts, to be turned into bone by osteoblasts.
Animation screenshot from Physiology & Pathology.
The healing process may sound fairly simple, but there are a lot of things that can go wrong. If the bone isn’t aligned properly or if it isn’t immobilized for long enough, the repaired bone could end up bent, twisted, or shortened, resulting in pain and inflammation. This is known as mal-union. Basically, the bone grows back incorrectly.
Sometimes the fractured bone doesn’t fully knit back together at all. This is called non-union, and results in pain, instability, and possibly even unnatural movement or clicking at the location of the fracture. Usually, non-union is treated with surgery, which can involve bone grafts.
If the fracture site is exposed to bacteria—say the skin was broken in the injury that caused the fracture or bacteria crept in during surgery—infection of the bone tissue, called osteomyelitis, may occur. Its symptoms include pain and inflammation as well as fever and chills. It can also cause non-union of the fractured bone. Usually, antibiotics are used to treat osteomyelitis.
Now let’s talk about strains and sprains. A strain happens when a muscle or tendon overstretches and/or tears. This happens a lot with the muscles of the hamstrings and the lower back.
A sprain happens when a ligament overstretches and/or tears. In the ankle, this most commonly occurs in the anterior talofibular ligament (ATFL) and calcaneofibular ligament (CFL). For example, the image below shows a partial tearing of the ATFL—aka a grade 2 ankle sprain.
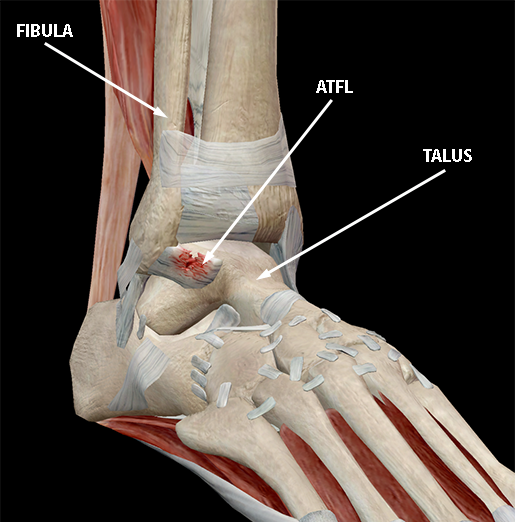 Image from Physiology & Pathology.
Image from Physiology & Pathology.
A grade 1 ankle sprain would involve slight stretching and some damage to the ligament, and a grade 3 ankle sprain would mean that the ligament has torn completely.
The traditional recommendation for treatment of sprains and strains is RICE (rest, ice, compression, and elevation), although some experts have contested the effectiveness of the “rest” and “ice” portions of the regimen. Medications like ibuprofen or aspirin can be used to reduce pain. All that being said, if you have a sprain or strain, the best plan of action is to follow the advice of the medical professionals caring for you.
2. Osteoporosis
Even in healthy, non-fractured bones, osteoclasts clear out old bone tissue and osteoblasts generate new bone tissue. Osteoporosis is a condition that arises when the ratio of old bone to new bone is thrown out of balance: more bone tissue is lost than is generated, leading to weak, brittle bones.
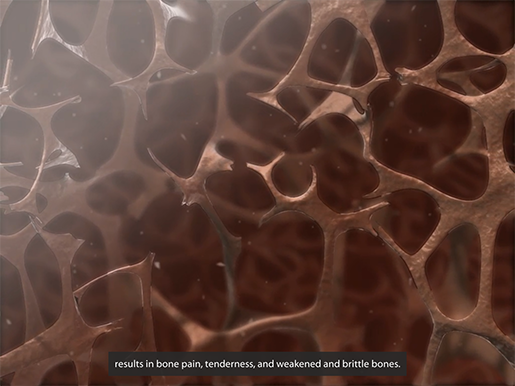 Animation screenshot from Physiology & Pathology.
Animation screenshot from Physiology & Pathology.
Osteoporosis typically doesn’t show obvious symptoms in its earlier stages, though back pain, height loss and/or a stooped posture may develop over time. Because osteoporotic bones fracture more easily, fractures are often how people first find out they have osteoporosis.
As people get older, their body slows down in its efforts to create new bone, so older people are at a greater risk for osteoporosis. There is a wide range of other risk factors as well. For example, women, especially those of white or Asian descent, are more likely to develop osteoporosis. If someone in your immediate family (a parent or a sibling) has osteoporosis, you’re also more likely to develop it. In addition, people with smaller builds have less bone mass in general, so they are at an increased risk of osteoporosis as well. Certain medications and illnesses may also cause bone loss, and therefore make osteoporosis more likely.
Here’s some good news: there are a lot of small lifestyle changes that can help people maintain good bone health. Making sure to get plenty of calcium and vitamin D can help your bones stay strong. A combination of strength training and weight-bearing exercise (even just walking!) is also helpful in that regard. Balance training can reduce the risk of falling, and maintaining a healthy weight decreases the risk of fractures. Doing these things won’t 100% prevent osteoporosis, but it never hurts to maintain a healthy diet and exercise regularly.
Medications called bisphosphonates are the most common osteoporosis treatment for people with an elevated risk of fracture.
3. Osteosarcoma
An osteosarcoma is a malignant tumor that originates in the bone tissue. They occur most frequently in children and young adults and are commonly found at the ends of long bones such as the femur, tibia, and humerus. One of the most dangerous things about this type of cancer is that it can spread to other areas of the body—that is, it can metastasize.
Symptoms of osteosarcoma include pain and/or swelling near a joint or bone, fatigue, anemia, and fracturing of weakened bone tissue. Because of these symptoms, most osteosarcomas are caught fairly early on (which is good, because the prognosis is usually better before the cancer has spread to other parts of the body). If a doctor suspects bone cancer after a physical examination, they will likely recommend further tests, which can include various imaging methods, biopsies, and lab tests.
 Illustration from Physiology & Pathology.
Illustration from Physiology & Pathology.
Osteosarcoma is usually treated with chemotherapy and surgery to remove the tumor. Surgeons do their best to spare the affected limb, but sometimes amputation of all or part of the limb is necessary.
4. Duchenne Muscular Dystrophy
Duchenne Muscular Dystrophy (DMD) is a genetic condition that causes the progressive weakening and degeneration of muscles. Around the world, about 20,000 new cases are diagnosed each year.
In DMD, a mutation of the DMD gene causes a lack of the protein dystrophin in muscle cells. Because this gene is on the X chromosome, the condition typically occurs in males. The absence of dystrophin is a problem because without dystrophin to support it and connect it to actin filaments inside the muscle fiber, the sarcolemma—the membrane surrounding muscle fibers—can easily tear.
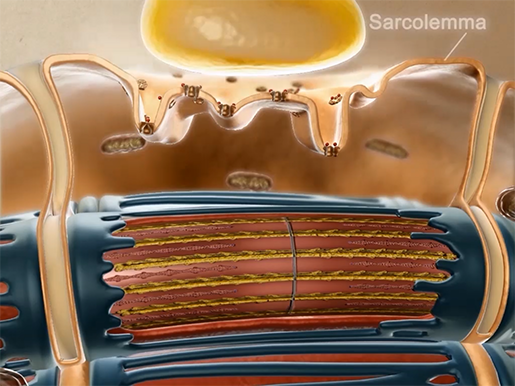 Animation screenshot from Physiology & Pathology.
Animation screenshot from Physiology & Pathology.
This allows extra calcium ions—that is, more calcium ions than are normally involved in muscle contraction—to enter the muscle fiber. The excess of calcium ions triggers the release of enzymes that damage the actin and myosin filaments within the muscle fiber.
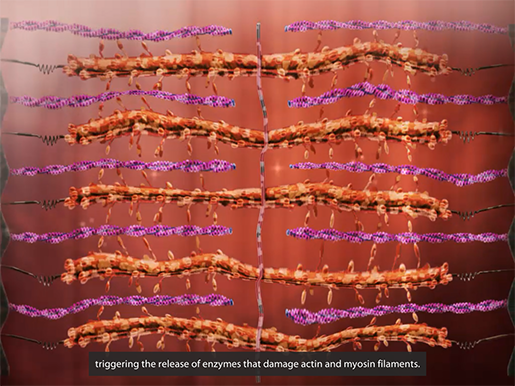 Damaged actin and myosin filaments. Animation screenshot from Physiology & Pathology.
Damaged actin and myosin filaments. Animation screenshot from Physiology & Pathology.
Damage to these fibers impairs the muscle’s ability to contract, and the muscle weakens. Eventually, muscle fibers are replaced by scar tissue and fat.
The symptoms of DMD typically occur in early childhood, around the age of 2 or 3. Muscle weakness begins in the shoulders, upper arms, hips, and thighs, which can lead to young children with DMD having trouble learning to sit, stand, and walk. As the child gets older, this muscle weakness spreads to the rest of the body, including the heart and respiratory muscles. This can result in severe complications, such as pneumonia (which can lead to respiratory failure) and cardiomyopathy (which can lead to heart failure).
Though some individuals with DMD can now live into their 30s (and even their 40s or 50s), the condition still proves fatal. Currently, there is no cure, though researchers are hard at work, developing “complementary therapies that could replace dystrophin, protect the muscle from injury, and/or promote muscle repair and regrowth.” The treatments available now are focused on improving muscle function (via physical therapy and special braces), maintaining cardiovascular and respiratory function (via medication and assisted ventilation), and helping people with DMD perform everyday tasks (via occupational therapy).
5. Neuromuscular Disorders
“Neuromuscular disorders” is a broad term that covers numerous different conditions. What all of them have in common is that they impair the ability of the nervous system to interact with the muscular system.
One of the nervous system’s many functions is to issue commands to the body’s muscles. When the central and peripheral nervous systems are functioning normally, signals from the brain travel down the spinal cord and out through the peripheral nervous system’s motor neurons. These neurons interface with muscles at neuromuscular junctions and release the neurotransmitter acetylcholine, kicking off muscle contraction.
In myasthenia gravis, a neuromuscular disorder characterized by severe muscle weakness that worsens after activity and improves with rest, the immune system interferes with this communication. Antibodies block, alter, or destroy the receptors for acetylcholine at neuromuscular junctions. Fortunately, there are several effective therapies available for myasthenia gravis, and most people with the disorder have a normal life expectancy.
Neurodegenerative disorders affecting particular regions of the brain and/or particular types of neurons can affect communication between the nervous system and the muscles.
In ALS (amyotrophic lateral sclerosis), for example, the death of motor neurons at first causes muscle weakness and eventually leads to the loss of the ability to walk, speak, swallow, and breathe. ALS is a devastating and deadly disease—life expectancy after diagnosis is usually between 2 and 5 years. Scientists are currently engaged in researching a cure, as well as ways of improving quality of life for people with ALS.
Though Parkinson’s disease doesn’t directly affect motor neurons, it does cause the death of dopamine-producing neurons in the substantia nigra, which interferes with a neural pathway in the brain that facilitates movement. There is not yet a cure for Parkinson’s disease, but there are medications that can help with managing symptoms.
These conditions are just a small sample of the wide range of musculoskeletal pathologies that extends from temporary injuries to debilitating and even fatal disorders.
If you’d like to learn more about the normal functioning and pathologies of the muscular and skeletal systems, check out Physiology and Pathology (now available for iOS and Android).
Be sure to subscribe to the Visible Body Blog for more anatomy awesomeness!
Are you an instructor? We have award-winning 3D products and resources for your anatomy and physiology course! Learn more here.



