5 Deadly Pandemics of the Past and What We Can Learn From Them
Posted on 5/20/20 by Laura Snider
Whether caused by bacteria, viruses, or other malicious microorganisms, disease has been a part of human life since there has been human life. That’s especially true now, when most of us have been impacted by COVID-19 in one way or another.
Today, we’re going to talk about some of the pandemics that preceded the one in which we currently find ourselves. The story of each is interesting in its own right, but the pandemics of the past can teach us a lot about the interactions between science and society.
By studying the bubonic plague, we gain insight into the origins of quarantine. Cholera clearly shows the importance of sanitation in our cities and gave the “father of modern epidemiology” his start. More recent pandemics—the Spanish flu, SARS, and MERS—demonstrate the importance of communication and infrastructural preparedness in fighting disease.
What is a pandemic?
First things first. Before we start on the history, let’s talk about what exactly a pandemic is.
A pandemic is defined as a disease “prevalent over a whole country or the world”—it’s what happens when a disease outbreak, or epidemic, grows to a worldwide scale. Today, the World Health Organization is the authority that declares when an epidemic has escalated to a pandemic. For example, on March 11, 2020, they announced at a news briefing that COVID-19 had become a pandemic.
1. The Bubonic Plague, or "Black Death" (1346-1353)
If I asked you to imagine a plague, my guess would be that you’d picture something like the “bring out your dead” scene from Monty Python and the Holy Grail: a bleak and filthy medieval cityscape where everyone is sick or dying. The fact that the bubonic plague devastated most of the world back in the 1300s, killing 25-50 million people in Europe alone, certainly cemented its place in popular culture as the archetype for devastating disease.
While it’s true that medieval medical science was nowhere near advanced enough to prevent such massive casualties, did you know that the bubonic plague led to the birth of the practice of quarantine as we know it? Let’s check out the facts.
Bubonic plague is caused by the bacterium Yersinia pestis (Y. pestis for short), and this microorganism can spread to humans when they are bitten by fleas who have fed on infected small mammals, such as rats, mice, and prairie dogs. Direct exposure to the blood of an infected animal can also spread the disease. Rats are typically blamed for the spread of the bubonic plague in the 1300s, but fleas and lice likely fed on infected humans and spread the infection that way as well.
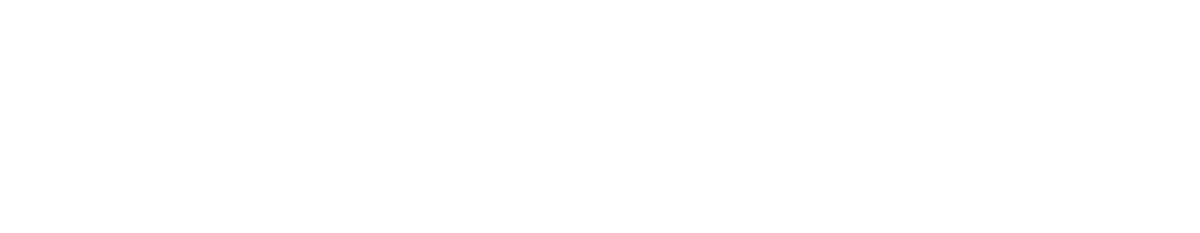
The bubonic plague gets its name from its most prominent symptom: “painfully swollen lymph glands that form pus-filled boils called buboes.” Buboes typically form in areas with a high concentration of lymph nodes: the neck, groin, and underarms.
The lymphatic nodes and vessels of the neck and upper torso, including the underarm (axillary) area. Image from Human Anatomy Atlas.
Other symptoms include “fever, chills, headaches, shortness of breath, hemorrhaging, bloody sputum, vomiting and delirium.” Without treatment, the survival rate is around 50%.
Although bubonic plague has historically been the most common form of plague caused by Y. pestis, infection by this bacterium can result in two other types of plague: pneumonic (which spreads via respiratory droplets and primarily affects the respiratory system) and septicemic (in which the bacteria multiplies in the bloodstream).
Today, there are occasional cases of bubonic plague, but they are few and far between. We also have strong antibiotics that can be used to treat it when it does crop up.
People in the 14th century, however, were not so fortunate. The Black Death swept through China, India, Persia, Syria, and Egypt in the early 1340s and arrived in Europe via its ports several years later. In 1347, infected sailors left the Genoese outpost of Caffa (located on the Black Sea) and landed in Constantinople (Istanbul), Sicily, and Marseille, carrying the plague with them. Similarly, a different strain of Y. pestis entered Italy through Genoa in 1348.
Over the next few years, the bubonic plague spread throughout Europe, reaching as far as Scotland and Norway. By the time 1353 rolled around, Europe had lost around half of its population. To add insult to injury, the plague would resurface several times in the next few centuries—the Great Plague of London in 1665 is a particularly notable resurgence.
So where does quarantine come in? The bubonic plague resulted in several measures to keep sick or potentially sick people isolated. In port cities like Venice, incoming ships were required to stay anchored for forty days (quaranta giorni) before their crews could enter the city. This period of time was referred to as a “quarantino,” which is the source of the English term “quarantine.”
Why forty days? Historians think that the number forty held cultural and religious significance for the people of medieval Europe. Fortunately, forty days was longer than the period of incubation for the bubonic plague, so these early quarantines did help at least a little, and they resulted in policies that persisted after the main wave of plague had passed.
Similarly, the port city of Ragusa (modern day Dubrovnik, Croatia) passed a law in 1377 stating that “those who come from plague-infested areas shall not enter [Ragusa] or its district unless they spend a month on the islet of Mrkan or in the town of Cavtat, for the purpose of disinfection.”
Venice and Ragusa also established plague hospitals, whose patients were exclusively people suffering from plague. These hospitals were also separated from population centers. In Ragusa, the plague hospital was set up on the nearby island of Mljet, and in Venice, there was a plague hospital on the island of Santa Maria di Nazareth.
Quarantines may not have eradicated the plague, but they certainly proved to be helpful in protecting port cities like Venice and Ragusa. The practice of quarantine showed the beginnings of society’s understanding that it was important to keep potential carriers of illness isolated from people who were well—even if sailors entering a port appeared healthy, they would have to isolate anyway if they were coming from an area where there was plague.
2. Cholera (1817-)
The story of the cholera pandemics of the 19th century shows the beginnings of modern epidemiological practices as well as a growing understanding that contaminated food and water can be vectors for disease. Also, it’s got John Snow in it—and this John Snow, unlike the Game of Thrones character, happened to know a lot.
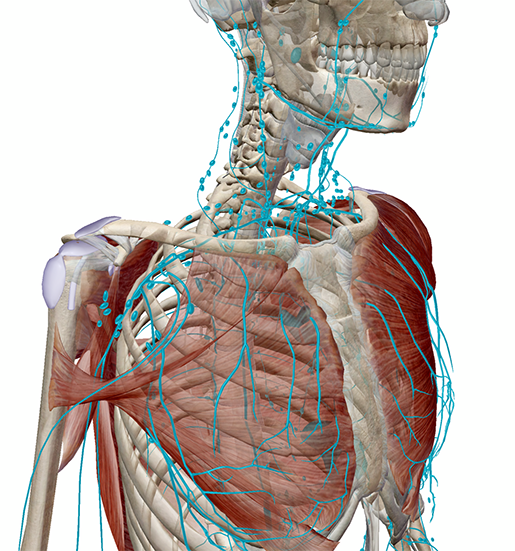
Cholera is a disease caused by certain strains of a bacterium called Vibrio cholerae. V. cholerae produces a toxin that makes cells in the lining of the intestines release too much water, causing rapid dehydration and fluid-electrolyte imbalance. Symptoms include vomiting, diarrhea, and leg cramps, and if untreated, cholera can lead to death in only a few hours. People can contract cholera if they consume food or water that has been contaminated by the feces of an infected person.
The mucosa is the innermost layer, or lining, of the small intestine. Image from Human Anatomy Atlas.
While today cholera can be treated with IV fluids and antibiotics, or even prevented with a vaccine, it proved to be devastating to people all over the world in the 19th century.
The first cholera pandemic occurred in 1817. It began with contaminated rice in India, and from there it spread throughout the Middle East and Asia via trade routes. By 1824, the pandemic had subsided, but a second one was close on its heels, beginning five years later This time, though, cholera spread as far as Europe and the Americas. This second pandemic didn’t “officially” end until 1851, which meant a long twenty years or so of on and off cholera outbreaks in various countries.
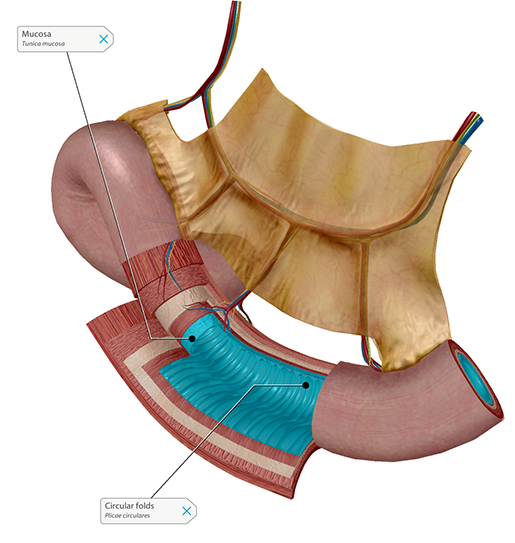
1852-1859 saw the third and deadliest cholera pandemic. In 1854, a British scientist and early epidemiologist named John Snow tracked cases of cholera in London and figured out that a particular well was the epicenter of the outbreak. Snow interviewed locals and created a map which helped him to trace the cholera cases back to the water supply.
 John Snow’s original map of cholera cases in London. Public domain image from Wikimedia Commons.
John Snow’s original map of cholera cases in London. Public domain image from Wikimedia Commons.
In addition, although the germ theory of disease hadn’t been fully developed at the time, Snow’s conclusion that drinking contaminated water was making people sick challenged the commonly accepted “miasma” theory of disease transmission. He convinced local officials to remove the handle from the pump that drew water from the contaminated well and the number of cholera infections in the area drastically decreased.
Fun fact: 1854 was also the year in which the bacterium that causes cholera was identified by an Italian microbiologist named Filippo Pacini.
The fourth cholera pandemic occurred from 1863-1875, once again resulting in outbreaks in numerous countries. During the fifth pandemic, which lasted from 1881-1896, microbiologist Robert Koch (whose work proved foundational to establishing the germ theory of disease) studied V. cholerae and showed that cholera was caused by its presence in the intestines. By the time the sixth pandemic arrived in 1899, most of Western Europe and North America had improved public sanitation enough that they didn’t suffer many casualties, but between 1899 and 1923, many people in North Africa, Russia, the Middle East, and India died from cholera.
Though we’re technically in the midst of the seventh cholera pandemic, which began in 1961 in Indonesia, the overwhelming majority of cholera cases and outbreaks occur in nations without effective public sanitation systems.
As for the cholera epidemics of the past, they can teach us several things. First, they clearly demonstrate the importance of keeping drinking water far away from waste. The tracing of cholera back to its source during the third pandemic also represents a significant stride forward in epidemiological thinking and techniques.
3. The Spanish Flu (1918-1919)
The Spanish Flu is the 20th century pandemic people seem to have compared to the COVID-19 crisis the most. Why? There are a couple of parallels to consider. Although SARS-CoV-2, the virus that causes COVID-19, is not the same as influenza, both viruses spread via respiratory droplets. Also, we don’t yet have a vaccine for it SARS-CoV-2, much as the people in 1918 didn’t have any kind of flu vaccine. The Spanish Flu pandemic is also noted for having had two waves—an initial one in the spring of 1918 and a devastating resurgence in the fall of that year. Experts warn that if we’re not careful, this could happen with COVID-19 in 2020 as well.
Despite its name, the influenza pandemic that occurred in 1918 didn’t originate in Spain. The Spanish flu is referred to as such because journalists from Madrid were the ones who brought it to the world’s attention.
Like other strains of influenza, the Spanish flu caused respiratory symptoms, fever, chills, and fatigue. In the initial wave of infection in the spring of 1918, it led to pneumonia for some, but many others recovered fully.
How influenza enters the body.
The death toll wasn’t very high at first. However, one characteristic that set this flu apart from others was that it infected and killed people who were otherwise young and healthy—notably soldiers fighting in World War I.
It’s not clear where exactly the virus originated, but the first known case in the US was in March 1918 at Camp Funston in Fort Riley, Kansas. The disease spread quickly among soldiers, who were living and traveling in close quarters—36% of troops in the US Army and around 40% of individuals serving in the Navy were ultimately infected. In the US alone, 670,000 people lost their lives. Worldwide, the Spanish flu infected 500 million people and killed between 50 and 100 million people.
The second wave of the Spanish flu struck in the autumn of 1918, and it proved to be much more catastrophic than the first due to a mutation in the virus. Young, healthy people could be struck down in as little as 24 hours, their immune systems overreacting in a “cytokine explosion” that caused them to drown in fluid from their own lungs.The symptoms were horrific—physicians described their patients’ skin turning blue as they were gradually deprived of oxygen. There was a third wave of Spanish flu, but it wasn’t nearly as deadly as the second, and by the summer of 1919, the pandemic finally ended.
In many ways, the public health responses (or lack thereof) to the Spanish flu serve as useful cautionary tales. In lots of places throughout the US, the responses were nonexistent or provided too little, too late. One particularly prominent example is when, in September 1918, the city of Philadelphia held a huge Liberty Loan parade despite warnings from doctors that having so many people in close proximity to each other was a bad idea. Within 10 days, 1,000 Philadelphians had died and thousands more had been infected. This incident shows just how important it is for public officials and medical experts to work together in matters of public health.
4-5. SARS (2002-2004) & MERS (2012-2016)
SARS and MERS provide the closest parallels to COVID-19 for several reasons. First, SARS, MERS, and SARS-CoV-2 are all coronaviruses that passed to humans from animals—SARS passed to humans from the civet cat, and MERS from dromedary camels. In addition, all three viruses were identified after patients were admitted to hospitals with severe pneumonia.
An article published by Peeri et al. in the International Journal of Epidemiology in late February provides a thorough explanation of the similarities and differences between the three viruses, as well as what those comparisons can show us about how best to handle a pandemic.
All three coronaviruses have a fever and cough amongst their symptoms, are known to cause pneumonia, and can be diagnosed by PCR (polymerase chain reaction) analysis of samples of respiratory fluids. The mode of transmission—respiratory droplets—is also the same across the three viruses. Additionally, although the mortality rate of COVID-19 is technically lower than that of SARS or MERS, the total number of cases of COVID-19 is much higher.
A virtual tour of the respiratory system—the body system most affected by SARS, MERS, and COVID-19. Video footage from Human Anatomy Atlas.
Much as with COVID-19, part of the reason SARS spread globally was that the outbreak wasn’t caught particularly early, and there was not enough protective gear immediately available for the general population to help slow the spread of the disease. Essentially, SARS caught healthcare systems off guard.
MERS did not spread as far as SARS or COVID-19, partially because the risk of human to human transmission was lower. However, the spread of MERS showed how issues maintaining infection control methods could impede the ability of people in certain areas to fight the disease. Many areas in the Middle East had issues maintaining physical barriers between patients, keeping patients in negative pressure rooms, and adhering to proper sanitation measures.
On a more positive note, the rapid and effective public health response to the MERS outbreak in South Korea provides a good example of the success of collaboration with the WHO and “intensified public health measures, including contact tracing, quarantine and isolation of all contacts and suspected cases.”
Ultimately, SARS, MERS, and the various responses to COVID-19 remind us of the importance of timely and transparent communication between governments, public health officials, and the public. They also show us that it can be dangerous when a country’s health infrastructure isn’t prepared to handle a large-scale crisis: having an adequate supply of protective gear for healthcare workers, as well as the public, is a valuable weapon against diseases that spread by close person to person contact.
What looking back at the pandemics of the past shows us is that disease is a formidable opponent, whether our technology and level of medical knowledge is medieval or modern. It’s important for humanity’s past experiences to inform its present and future ones.
Be sure to subscribe to the Visible Body Blog for more anatomy awesomeness!
Are you an instructor? We have award-winning 3D products and resources for your anatomy and physiology course! Learn more here.
Additional Sources:
- Business Insider: 11 ways pandemics have changed the course of human history
- The Conversation: A brief history of the coronavirus family – including one pandemic we might have missed
- CDC: MERS FAQ
- CDC: SARS Basic Factsheet
- The Guardian: How humans have reacted to pandemics through history – a visual guide
- History.com: Pandemics that Changed History
- LA Times: From the Black Death to AIDS, pandemics have shaped human history. Coronavirus will too.
- NPR: What the 1918 Flu Can Teach Us About Handling Today's Pandemic
- World Economic Forum: A Visual History of Pandemics